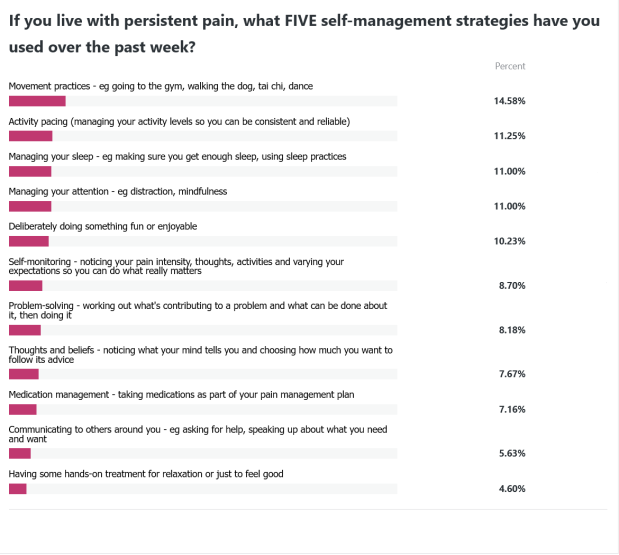
When I carried out my informal survey of the pain self-management skills people had used in the past week, there were no real surprises. Movement, activity management (pacing – and I will have more to say about this in a couple of weeks!), sleep, attention management and doing something fun were all at the top of the list. Others were lower down and while they don’t get to shine as much, I’m not so sure they are as seldom used as this wee survey suggests.
At the bottom of the list is having hands-on treatment for relaxation or to feel good. OK, perhaps understandable because the whole ongoing debate about hands-on or hands-off therapy is nowhere near resolved. (FWIW I enjoy a massage, there’s something special about being touched nicely by someone who cares about how it feels, but I’m less convinced that hands-on therapy does much more than this. Just feeling nice is, on the other hand, a pretty darned good thing if you’re generally sore.)
The next to last is communicating your needs to others around you. A couple of thoughts here.
First one is that being open and honest about what you need doesn’t come easy to many of us. I think it’s even more difficult if you’re worried that people think you’re well but you’re actually sore. There is stigma associated with asking for help. There is stigma with having an invisible chronic disability. Asking for help risks being denied that help or being rejected. Why would you do that when you’re feeling vulnerable as it is?
The second is that if you’ve been living with pain for many years, our own expectations (and of the people around us) are often recalibrated. That is, our lives adjust and people get used to what we can and can’t do. Initially, some of the people we care about or who are friends may fall away because we’re violating their expectations (we can’t do the things we used to) and lots of people I’ve listened to say they soon learn who their friends really are! Later, we build friendships with those who do understand the ‘new you.’ We also change what we expect from ourselves and find ways to do the things even with our altered capabilities. This means we don’t need to specifically ask for help in the way that this survey identified.
The early days of learning to live with pain involves so many changes, and communicating what we need can be amongst the hardest things to do. I can say, though, that it gets a little easier over time but for me it’s never my favourite thing.
The approach I use is based on some really old ‘assertiveness’ training ideas. First, what not to do…
There’s the pussy-footing approach where we just hint or indirectly communicate what we want. This is often accompanied by frustration and what some people describe as ‘passive-aggressive’ behaviour. You know the thing: huffing because someone didn’t offer to help with a thing. Rolling the eyes. Going quiet and giving people the silent treatment. It’s not a great strategy because none of us are mind-readers! Loads of opportunity for mixed messages or being ignored, and really it’s a great way to undermine an honest and open relationship. The aggressive reaction after a period of being passive comes out of the blue and the person on the receiving end doesn’t know what’s hit them.
The other option is clobbering. You know, the old shouty, ‘I’m right and you’re wrong‘ stance, where again, the other person doesn’t know what’s hit them. It might not even be shouty – it’s the sense that the other person ought to know what you need, and your needs are always top priority, even if you haven’t said anything about what it is you want. Not a great way to win friends and influence people – yet quite common in some areas of social media, and yes, in the workplace.
If neither of these two options is all that great, what’s left? I call it being straight up. It’s calmly and clearly saying what you want. Not apologising, not expecting, just asking or stating your needs.
There is a script or kind of template that can help communicate in this way. It’s called the DESC and I have no idea where it originated. I can tell you that it’s a reasonable formula but as ever, needs to be individualised and tailored for context.
D = describe the current situation or status quo. Something like ‘I’m trying to move this box from here to here.’
E = explain what’s not working about the situation. Maybe ‘I’m having trouble getting a decent grip on it because my fingers are sore and weak.’
S = state your request simply, and clearly. ‘Can you help me by holding on to the other end while I move the box?’
C = indicate the consequences, or how this will help. ‘Then I can get out of your way, the box will be where I need it, and I’ll be happy!’
Even quite complex interpersonal situations can be managed using this strategy.
‘I’m trying to clean the benches [D], but there are heaps of dirty coffee cups on it and I don’t think I should have to clear up after everyone [E]. Would you all do your own coffee cups please? [S] Then I can get on and tidy up quickly [C].’
‘I’ve been having a hard time sleeping recently [D] but you’re lying flat on your back snoring and it’s keeping me awake [E]. If I poke you and tell you to roll over, would you do that? [S] Then I’ll get some sleep and be a much less grumpy person [C].’
You can use this approach in lots of different settings – the important thing is to remember that the other person also has rights and responsibilities, and to be respectful. They may say no!
Here are a few sites with some simple tips and worksheets:
Therapist aid – click
Verywell Mind – click
Skillset – click
And just in case you think this is a 70’s chick being all retro, here are some research papers investigating assertive communication for your reading pleasure!
Ashton-James, C. E., & Ziadni, M. S. (2020). Uncovering and Resolving Social Conflicts Contributing to Chronic Pain: Emotional Awareness and Expression Therapy. Journal of Health Service Psychology, 46(3), 133-140. https://doi.org/10.1007/s42843-020-00017-y
Swift, C., Hocking, C., Dickinson, A., & Jones, M. (2019). Facilitating open family communication when a parent has chronic pain: A scoping review. Scandinavian journal of occupational therapy, 26(2), 103-120.
Braverman, M. T., Volmar, K. M., & Govier, D. J. (2023). “The Pain Doesn’t Have to Control You.” A Qualitative Evaluation of Three Pain Clinics Teaching Nonopioid Pain Management Strategies. American Journal of Health Promotion, 37(2), 210-221.
Pasini, I., Perlini, C., Donisi, V., Mason, A., Schweiger, V., Secchettin, E., … & Del Piccolo, L. (2023). “INTEGRO INTEGRated Psychotherapeutic InterventiOn” on the Management of Chronic Pain in Patients with Fibromyalgia: The Role of the Therapeutic Relationship. International Journal of Environmental Research and Public Health, 20(5), 3973.
